Throughout the years, tons of “wonder foods” have come and gone within the health community, based on a mixture of legitimate science and hype (remember goji berries? Maca root? Coconut oil? Flaxseed? Chia? Kale?). Now, a new contender is here for the superfood crown: resistant starch, especially in the form of raw potato starch. If you haven’t encountered enthusiastic advice to add potato starch (just stirred into a glass of cool water, yum?!) to your diet in order to treat all manner of ills, you probably will soon!
Resistant starch is a type of highly-fermentable insoluble fiber. Unlike most starches, resistant starch isn’t fully broken down in your small intestine. It “resists” the action of your digestive enzymes because of its molecular structure; and instead of being a source of slow-burning carbohydrates for you, it becomes food for specific types of bacteria in your colon (which ferment it to produce beneficial short-chain fatty acids like acetic acid, propionic acid, and butyric acid).
There are four main categories of resistant starch:
- RS1: starch that resists digestion because it’s trapped by intact plant cell walls (in legumes, grains, and seeds)
- RS2: starch that’s protected from digestion because of its molecular structure, and only becomes accessible to human digestive enzymes after being cooked (this one’s found in raw potatoes, green bananas, and raw plantains)
- RS3: also called “retrograded starch,” which forms when you cool down certain starchy foods after they’ve been cooked (such as potatoes, rice, and other grains)
- RS4: chemically modified starches that don’t occur in nature, but are created to resist digestion
If you’ve read my Fiber Manifesto, you already know that I’m a big fan of insoluble fiber for the host of benefits it provides. Fiber in general has been linked to reduced risk of diabetes, heart disease, and multiple cancers. It reduces inflammation, regulates hormones, and helps protect against many gut pathologies. And looking at the research on resistant starch in particular, it’s not hard to see why it’s becoming so heavily promoted as a supplement, especially in the Paleo community. Both human and animal studies have confirmed a number of legitimate benefits, including improved insulin sensitivity (and lower blood sugar responses after high-carb meals), reduced hunger/better satiation, improved blood lipids, and even better immunity (due to the influence of resistant starch on immune cell production and inflammatory compounds in the gut).
Sounds pretty great, right? Let’s toast with our glasses or potato starch stirred into water!
Er, or not. There’s another side of the resistant starch story that hasn’t received as much airtime: the consequences of supplementing with an isolated starch, rather than eating resistant starch as it naturally occurs in whole foods (mixed with other compounds that all work in concert). It turns out that, while whole food sources of resistant starch may be a health boon to the body, supplementation of concentrated sources of resistant starch—which is becoming all-the-rage in the low-carb, ketogenic diet, alternative health and primal/Paleo communities—isn’t such a good idea.
Let’s evaluate resistant starch supplementation objectively by turning away from the hype and instead looking at the science.
Effects of Isolated Resistant Starch: Location, Location, Location
As already mentioned, an array of studies prove that resistant starch provides tremendous benefits to our health. In addition to some of the more overt effects, like improved blood sugar regulation and cardiovascular disease risk factors, resistant starch can improve general health in more subtle, yet perhaps more profound, ways. For example, resistant starch can help increase absorption and bioavailability of many essential minerals from the diet, including: calcium, magnesium, zinc, iron and copper. Of course, other kinds of fiber can do this too, but this is likely one reason why supplementation with resistant starch can protect bone density during weight loss and positively impact the immune system.
Yet, multiple studies have highlighted the importance of consuming resistant starch in combination with other types of fermentable carbohydrate. This is important because these studies demonstrate the necessity to focus on whole food sources of resistant starch rather than jumping on the bandwagon with a supplement focus.
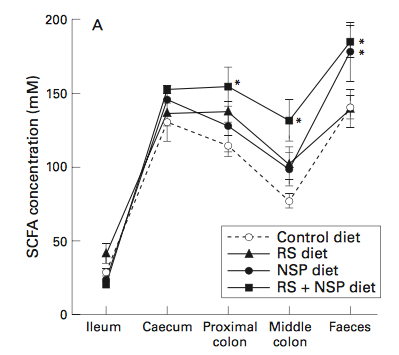
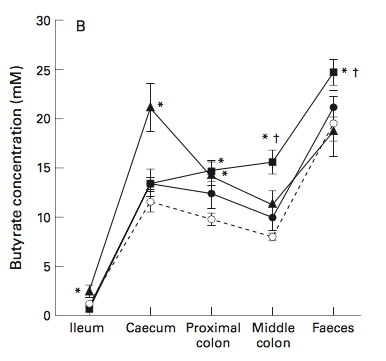
One study on pigs (whose large bowel is similar enough to humans’ to make the results worth reading about!) found that RS2 alone gets rapidly fermented in the proximal (beginning) part of the colon, but fails to reach further down into the distal (lower) colon. That’s bad news if we’re trying to achieve maximum cancer protection: the lower parts of the colon are where tumors occur the most often, and flooding the area with plenty of butyrate (produced by bacterial fermentation of resistant starch) can help inhibit the growth and differentiation of colon cancer cells.
But, in that same study, adding wheat bran (a soluble non-starch polysaccharide) to the pigs’ diet nearly doubled the amount of resistant starch getting fermented between the lower colon and feces. Basically, the bulk from the wheat bran helped carry fermentation further through the colon, spreading cancer-protective butyrate in the process (and providing some other perks along the way, like lower ammonia concentrations—something we don’t see in studies that use RS2 alone).
From: Govers M, et al. “Wheat bran affects the site of fermentation of resistant starch and luminal indexes related to colon cancer risk: a study in pigs.” Gut. 1999 Dec; 45(6): 840–847.
Another study, this one on humans, found something similar when wheat seed (RS1) was added to supplemental RS2 (in the form of green banana flour and high-amylose maize). The addition of wheat seed helped spread fermentation throughout the entire colon, as indicated by a decrease in fecal pH (which is a good thing!). In contrast, nearly all studies using RS2 on its own (from potato starch, high-amylose maize, and other sources) fail to show that fermentation reaches anywhere other than the very upper part of the colon.
So, does that mean you should add wheat to your diet to boost your gut health and cut your disease risk? No way! What these studies demonstrate isn’t that we should tinker with the effects of one isolated carbohydrate by adding another isolated carbohydrate on top of it, but instead, that resistant starches work in harmony with other dietary components to exert their full benefits. That’s another point in favor of eating resistant starch in whole-food form, since it already comes packaged with a variety of soluble and insoluble fibers (not to mention essential vitamins, minerals, and phytochemicals!) to keep your gut (and the rest of you!) healthy.
The Problem of Selectively Feeding Certain Bacteria
Another concern with aggressively supplementing with resistant starch (especially potato starch) is what happens to the composition of your gut microbiome. Different strains of bacteria have specific substrates they like to munch on, and while some are happy to dine on RS2, others prefer different forms of fiber. When we consume unnaturally high (e.g., supplemented) levels of one type of resistant starch (or one type of any fiber), we risk selectively feeding certain strains of bacteria while lowering the proportion of other beneficial kinds. Even beneficial probiotic strains of bacteria can overgrow, and this is especially a concern when this comes at the expense of microbial diversity—while much remains unknown about the optimum gut microbiome, one thing we know for sure is that a diverse microbiome is a resilient and healthy one.
A great paper examining this effect is from 2014, titled “Impacts of plant-based foods in ancestral hominin diets on the metabolism and function of gut microbiota in vitro.” In this study, a raw potato diet (RS2) caused human-derived fecal communities to show a major rise in Bacteroides and Eubacterium rectale (beneficial bacteria that thrive on RS2), due to the diet over-feeding them with their preferred food source. But, the raw potato diet also suppressed levels of bifidobacteria and lactobacilli—two types of beneficial bacteria that favor RS3 over RS2 and which enjoy other fiber types like inulin. For people supplementing with potato starch, or other isolated resistant starches (and especially at the expense of a diet that includes varied fiber sources), we might expect to see a similar change in microbiome composition, including a loss of certain bacteria that typically benefit our health.
Hypothetically, if you’ve had a stool test to analyze your gut microbiome, this property of resistant starch could be exploited to produce rapid correction of certain undesirable bacterial genus patterns with a short-term supplementation course. Certainly, some practitioners are using potato starch supplementation as one tool in an arsenal to correct gut dysbiosis. Caution is advised even with medically-supervised resistant starch supplementation however (read on for more on why whole foods sources of resistant starch are still a preferable strategy), and I encourage detailed conversations with your practitioner about whether or not this is the best approach for you.
There’s another concern for anyone with gastrointestinal symptoms. Even proponents of resistant starch supplementation caution its use for those with Small Intestinal Bacterial Overgrowth (SIBO). Although, let’s be clear: how resistant starch may exacerbate SIBO has never been evaluated in a scientific study. It remains unknown whether resistant starch could propel an overgrowth of bacteria higher up the digestive tract by providing such a highly fermentable substrate where microbial density is supposed to be only a fraction of what it is in the large intestine. However, studies in both dogs and humans show that resistant start is fermented by bacteria in the ileum (the last segment of the small intestine before the large intestine), producing mainly butyrate and acetate short-chain fatty acids. So, while this “caution” has yet to be scientifically validated, it is certainly possible.
How Resistant Starch Enhances Tumor Growth
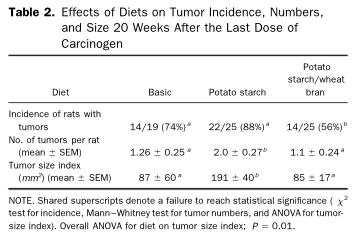
Now, for something a little more alarming. Several studies have demonstrated that, after exposure to a carcinogen, RS2 can actually enhance tumor growth (if it’s not accompanied by other forms of dietary fiber). Yikes, right? One study using a rat model of colorectal cancer found that raw potato starch supplementation led to larger and more frequent tumors, compared to a low-resistant starch control diet. (After 20 weeks, 88% of the rats eating potato starch had tumors, compared to 74% of the rats on a control diet, and their tumor size averaged 191 mm2 compared to 87 mm2 on the control diet.) Here’s the kicker though: when the rats were given potato starch plus wheat bran, those tumor-enhancing effects were suppressed (only 56% of the rats got tumors and the average tumor size was back down to 85 mm2). In other words, a soluble fiber coupled with resistant starch seemed to counteract the increased tumorigenesis.

HealthMeans for a Healthy Gut
Another study using a mouse model had a very similar outcome. In this experiment, carcinogen-exposed mice were fed different diets enhanced with aspirin, two forms of RS2 (raw potato starch and high-amylose corn), or a conventional rodent chow diet. Mice receiving the resistant starch had a significantly higher number of intestinal tumors than mice on any of the non-RS diets. (Interestingly, the addition of aspirin suppressed that effect—even though aspirin alone didn’t appear to have any anti-tumor properties.) And yet another rat study found that resistant starch from either potato starch or high-amylose corn increased the absorption of a dietary carcinogen in the heterocyclic amine family—something humans are also exposed to.
Could this problem just be limited to rodents, though? While the majority of animal research does translate to humans, certainly not all of it does which is why studies in animals do need to be taken with a grain of salt. Unfortunately, in this case, it doesn’t look like we can get away with the “but that’s just in rats” justification to dismiss a scientific study. In a human study using controlled diets enriched with either RS2 (from high-amylose maize) or cornstarch, RS2 significantly increased the amount of DNA adducts in the colonic mucosa, which is a biomarker for the formation of colorectal cancer. The average number of adduct levels went from 2.69 during the study’s low-RS period up to 3.83 during the high-RS period. That points to the potential of certain forms of resistant starch having a tumor-enhancing effect rather than a tumor-protective effect.
Keep in mind, this definitely isn’t the same as saying “resistant starch causes cancer!” In these studies, a potent carcinogen was used to kick off the process of cancer initiation, and RS2 just served to promote growth once it had started. But, that’s still a potentially dangerous situation, and it should serve as a warning that supplementing with isolated resistant starch may carry unforeseen risks—especially if it’s not carefully balanced by other soluble and insoluble fibers.
More Benefits with Fewer Risks: Whole Foods!
There’s little doubt that resistant starches play a beneficial role in our diet, and can go a long way in supporting healthy intestinal flora. In fact, the reduction in resistant-starch-rich foods may be a major reason low-carbohydrate diets tend to alter the gut microbiome in unfavorable ways (along with reductions in other fermentable fibers). But, we need to be careful when generalizing the effects of resistant starch in its whole-food form (potatoes, root veggies, bananas, plantains, etc.) to its effects as an isolated supplement. Unfortunately, the way potato starch supplementation is currently touted, as a gut microbiome-enhancing substitute for eating a variety of vegetables and fruit, doesn’t look like a strategy that lives up to the hype.
So far, the science suggests that resistant starch, especially RS2, exerts the most benefits when consumed with additional fermentable carbohydrates, soluble fibers that add fecal bulk, and perhaps other dietary components that enhance its positive effects while counteracting its negative ones.
Does this mean that all you have to do is add your potato starch to a breakfast smoothie that contains spinach and berries too? The research so far can’t tell us what the threshold amount of resistant starch relative to other fibers and carbohydrates is for optimal benefits (and avoiding detriments). It’s likely that all of the negative effects of resistant starch supplementation discussed here are non-issues when potato starch is added to a diet already rich in a variety of vegetables and fruits (although, if you are eating a diet rich in a variety of vegetables and fruits, chances are good that your microbiome is doing well without additional supplementation). The bigger caution here is for those using potato starch as a substitute for vegetables and fruits in their diets.
The best solution? Eat resistant starch where it naturally occurs! Cooked potatoes (which contain RS2 and RS3, of course, there’s even more RS2 in cooked and cooled potatoes), raw green bananas, plantains, yams, and other root vegetables provide not only resistant starch, but also a variety of other fibers and micronutrients that benefit health. Raw potato starch may be convenient, but in the long run, it’s less likely to benefit your health than eating resistant-starch-rich whole foods.
Source: Article by Dr. Sarah Ballantyne, PhD (https://www.thepaleomom.com/resistant-starch-its-not-all-sunshine-and-roses/)